Multiple Sclerosis is the first cause of disability in young adults, especially in young women. It’s crucial that we make an early diagnosis because early treatment can improve the course of the disease.
Table of content
What is multiple sclerosis?
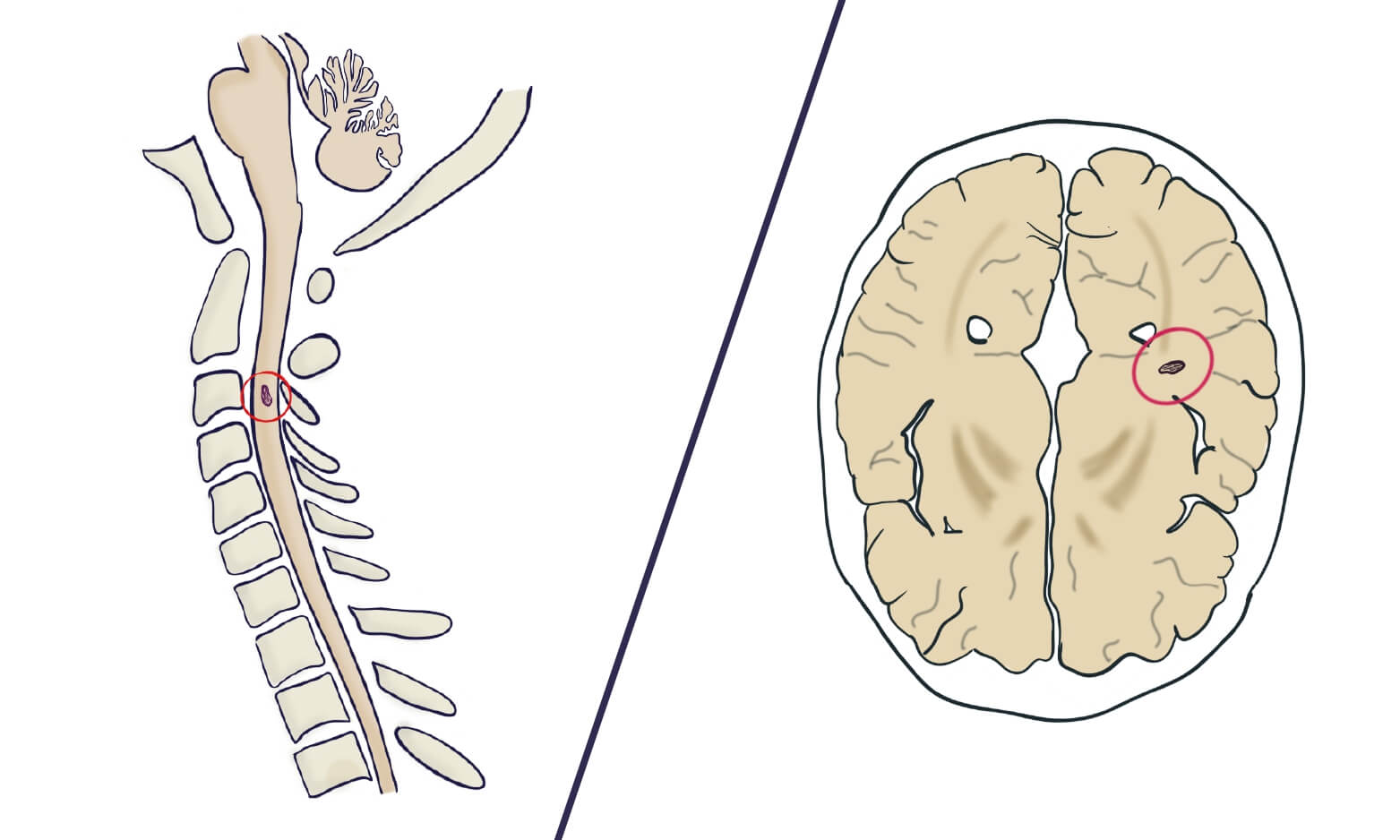
Multiple Sclerosis (MS) is a central nervous system disorder that causes loss of myelin in different areas of your brain and spine. This causes a bad transmission of your nervous signals, which causes neurological symptoms.
MS is more frequent in women but anyone can suffer it. Also, it usually affects young people, from 20 to 30 year old.
Sometimes, diagnosis multiple sclerosis can be tricky and it’s common that the diagnosis is delayed for many years. There are some people with unspecific symptoms that later find out they had MS. MS is not contagious and is not hereditary, although family members have a higher risk.
Risk factors for multiple sclerosis
We can’t predict who will suffer MS, but we know some risk factors that increase the risk. As we said young women are the most common patient. It’s also more frequent if you have family affected with MS.
Also, it’s interesting but there are some regions and some races with a higher risk. For example, the caucasian race has the highest risk and people living far from the equator have a high risk too, like scandinavian countries.
Having another autoimmune disease is another risk factor for MS, like if you have autoimmune hypothyroidism, psoriasis or type 1 diabetes.
Why does multiple sclerosis happen?
Your own immune system starts attacking your own cells. Our central nervous system works as an electrical system, where our neurons would be the wires. The spine sends signals from our brain towards our arms, legs and organs.
Our “wires” are surrounded by an insulating plastic cover: the myelin sheath. If our wires lose their cover, the signal will not travel so fast and will cause malfunction. This translates into different neurological symptoms like blurred vision, numbness…
During MS, your own immune system attacks your myelin sheaths by mistake. For a short time your body can repair the damage (through remyelination and plasticity), which can delay symptoms for months or years. However, if the attacks become more and more frequent, your body will not be able to repair all the wires.
There are 3 different types of multiple sclerosis
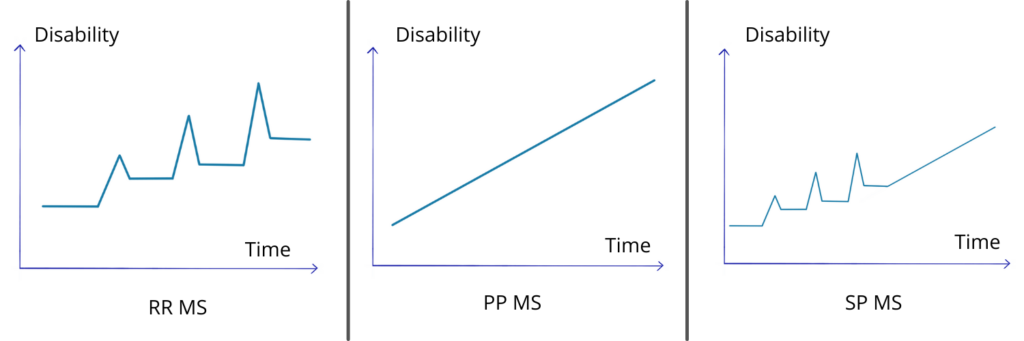
There are different types of MS, each of them with a different course. Some of them have relapses or attacks, after which they go back to virtually normal. Others have a more progressive course, with not so many attacks.
-
Relapsing-remitting multiple sclerosis (RR MS)
This is the most frequent course, specially in the beginning. 85% of patients have this type when they are diagnosed.
Relapsing-remitting MS consists of well defined attacks or relapses. The patient suddenly gets some neurological symptoms and then they recover, entering a period of stability.
The neurological symptoms sometimes disappear completely or there can be some residual deficit. However, there is no worsening between attacks. You can understand it better if you look at the graphic at the end of this section.
-
Clinically isolated syndrome (CIS)
It’s the first episode of neurological symptoms without any other conditions to explain them (there is no stroke, no brain tumor, etc).
It can be the beginning of MS, but in other cases, there are no more episodes and the patient never develops MS. After a first episode, you will get a brain MRI.
If your MRI shows typical MS lesions, there is a significant chance that you’ll develop MS (around 60-80%). If there are no lesions, chances are much lower (20%).
-
Primary progressive MS (PP MS)
There is a progressive worsening of symptoms, without significant “attacks”. There is no period of stability between relapses, because there are no relapses. 15% of patients have PP MS.
Sometimes, you can have progressive worsening and also some relapses in between. We call it progressive-relapsing MS, and it looks like a mix of RR MS and PP MS.
-
Secondary progressive MS (SP MS)
After some time, some of the patients with RR MS can transition to a progressive course. This is called secondary progressive MS: you start with “relapsing-remitting” and then go on to “progressive”.
Around 60% of patients with RR MS will turn into SP MS. Fortunately, early treatment can reduce this percentage or delay the progression.
– Active vs. not active
MS is active when there is a relapse going on: you have neurological symptoms at that moment. The period between attacks is considered not active.
– Worsening vs. not worsening
MS is worsening if there is more disability after an attack, if the symptoms didn’t resolve completely. If they resolve completely, we consider it not worsening.
Symptoms
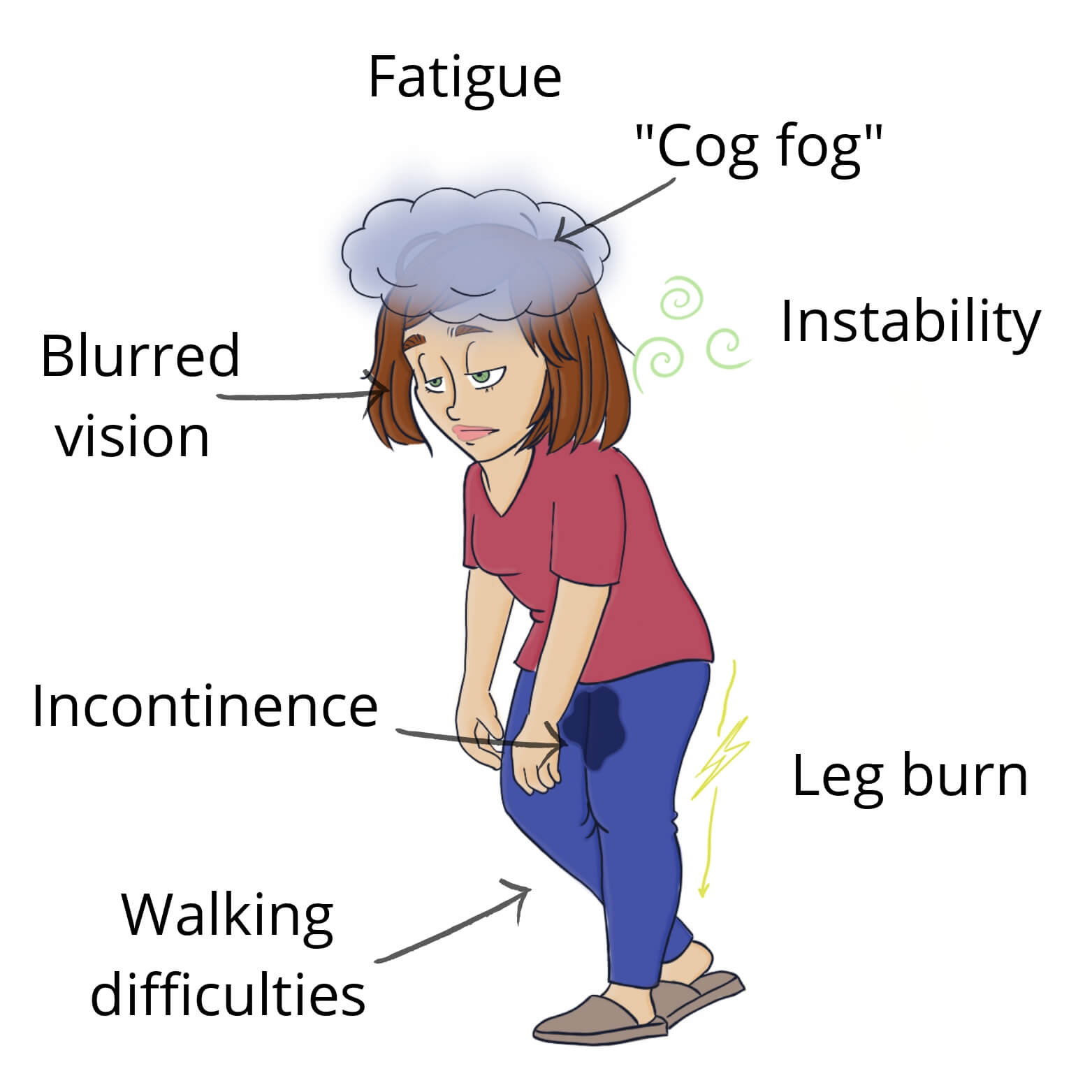
MS can cause a lot of different symptoms, depending where demyelination happens.
Fatigue is a very common symptom. Patients can have a hard time explaining it to the doctor as it is subjective (they have to believe you). However, many patients complain about it and it is a frequent cause of disability.
Blurred vision is another frequent one, because you can get optic neuritis, inflammation of the optic nerve, which causes blurred vision.
If lesions affects the cerebellum or the spine they can cause walking difficulties, sometimes in the form of spasticity (stiff muscles).
There is a phenomenom called “brain fog“. It’s when you lose your train of thought, forget your friend’s name, can’t express what you think… It’s also typical of multiple sclerosis and can be very frustrating because it’s a difficult symptom to understand from “outside”.
Some patients feel leg burn, pain, numbness…
There is a very upsetting symptom: bladder incontinence. Because MS patients are so young, they don’t expect it and they may feel stigmatized. It really is a pain in the a##. Tremors, lack of coordination and slurred speech are some other possible symptoms.
How to diagnose multiple sclerosis
Diagnosing multiple sclerosis early is critical because it leads to early treatment. And early treatment will reduce the number and severity of the relapses. It also will reduce the build-up of disability over time, slowing down the disease.
Multiple Sclerosis can be difficult to diagnose because there is not a definite test that will tell us if you have MS.
To diagnose MS first we need to exclude other causes that could explain the symptoms, like Lyme disease or lupus. Then we gather data that points towards MS.
These data come from clinical history, CSF analysis and MRI of the brain and spine. CSF = cerebrospinal fluid.
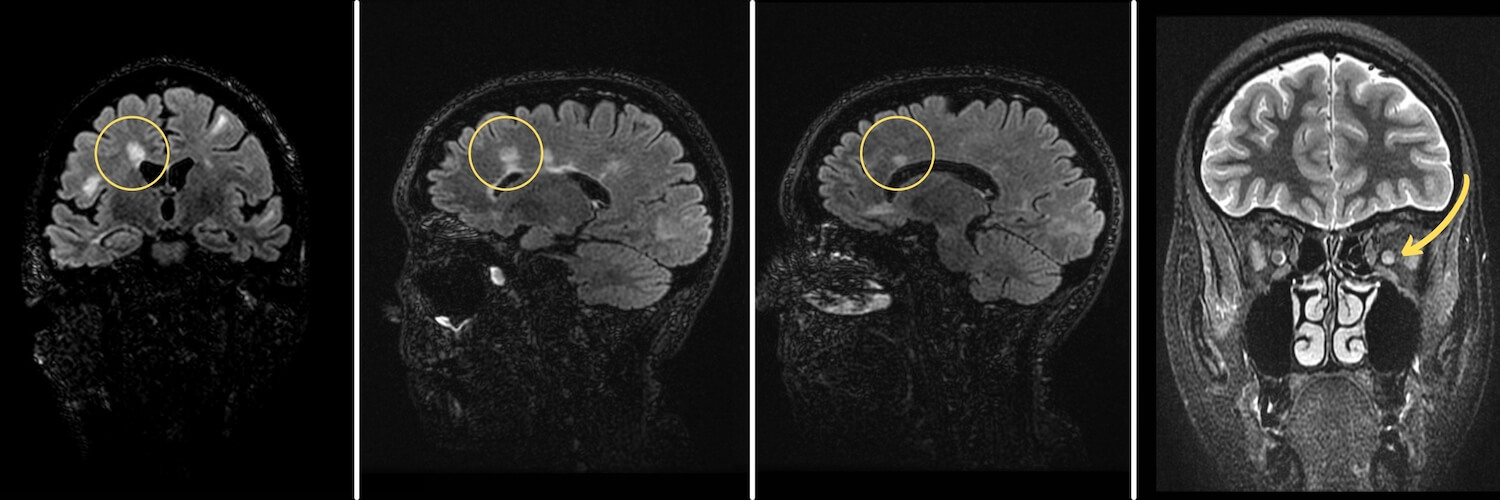
The MRI can help us prove “dissemination in space” (several regions) and “dissemination in time” (several episodes), which we need for the diagnosis. If a patient only has a single lesion, or had a single episode, that is not enough for the diagnosis.
Dissemination in space (DIS)
Dissemination in space means there are lesions in at least two different areas.
We can prove it clinically if the patient has burning sensation on their left hand and spasticity on their right foot, that may indicate lesions in two different areas of the brain.
However, it’s easier through MRI. MRI is a great tool for the diagnosis and follow-up of MS patients. There are well-defined regions on the MRI that allow us to determine whether there has been dissemination in space.
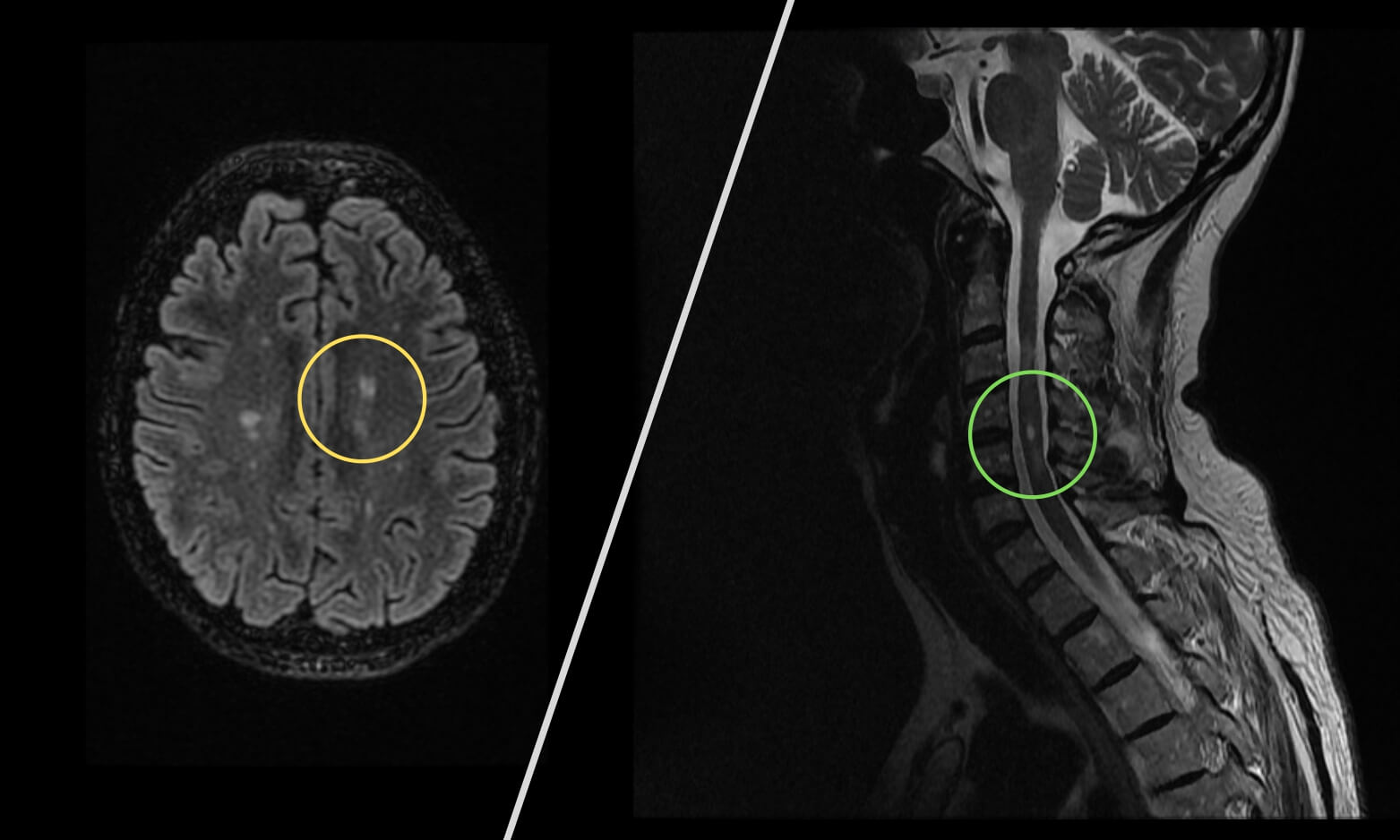
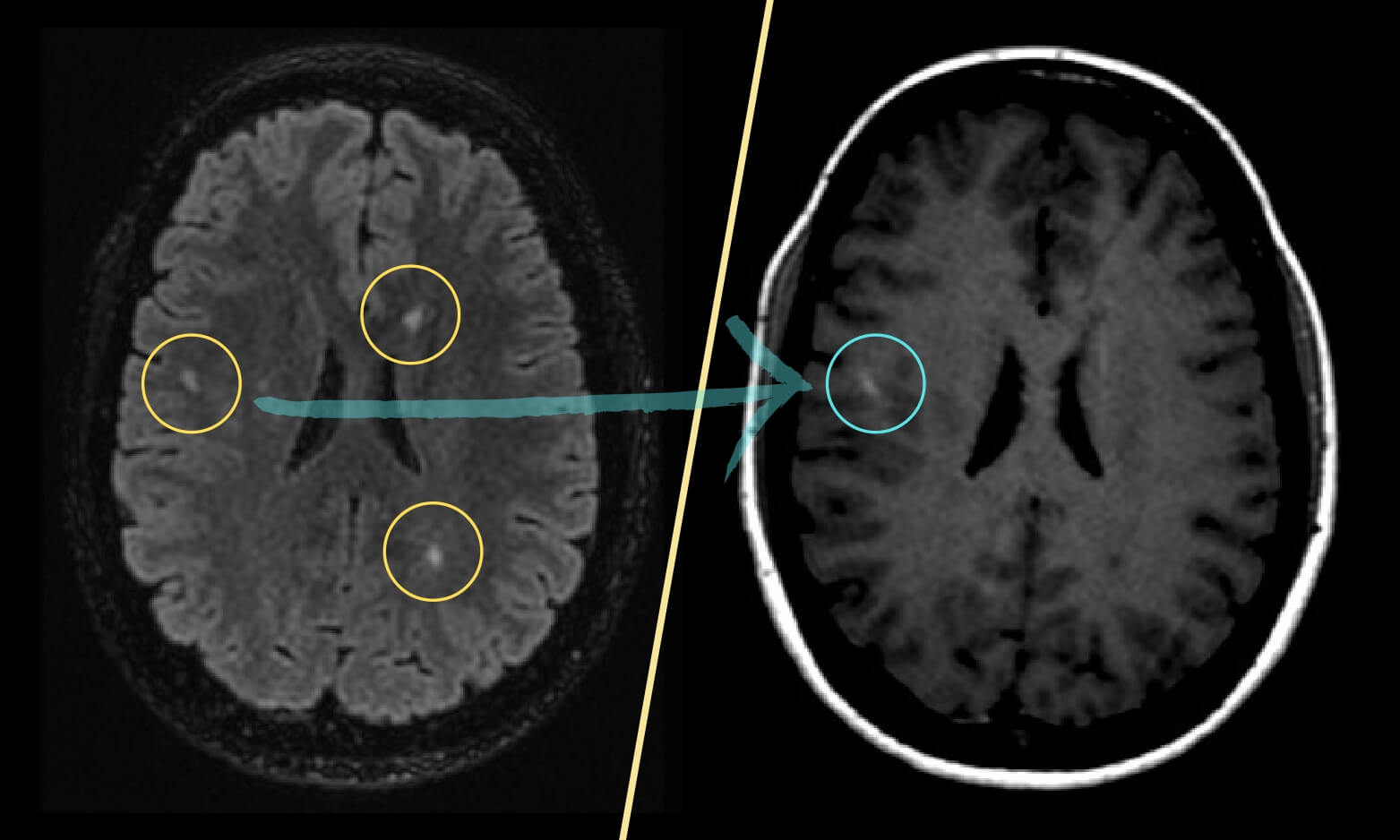
Dissemination in time (DIT)
The same with time, we need to prove there have been at least two different episodes. If the patient had a clear episode 6 months ago and a new one now, with a well-defined period in between, that’s dissemination in time.
MRI can sometimes prove it, too. In some cases, MRI can distinguish old lesions from new ones, if the later are “fresh“.
If we find old and new lesions in the same patient, there has been dissemination in time. This is great because the sooner we diagnose MS, the sooner we can start the right treatment.
How to treat multiple sclerosis
When we treat multiple sclerosis we have 2 goals:
- reducing symptoms
- and slowing down the disease.
How to treat MS symptoms
For every symptom that you suffer, there are some drugs to manage it. Your doctor will prescribe the combination that works best for you.
- For example if you have tremor, you may need some benzodiazepine, like clonazepam.
- If you suffer neuropathic pain, your doctor can prescribe some drugs like gabapentin.
- For spasticity and spasms, you may find baclofen useful.
How to treat MS attacks
During a MS attack, there is active inflammation causing damage. The fastest and most effective way to treat inflammation is with corticoids.
When we use them early, corticoids can reduce the symptoms.
If corticoids don’t work and your symptoms are severe, there is a more aggressive therapy: plasmapheresis. They connect your blood to a machine that “washes it“ and then returns it back to your body. It is used only as a last resource when corticoids don’t work, most patients don’t need it.
Disease modifying drugs (DMDs)
DMDs are drugs that can prevent or delay new attacks. If we start using these drugs early, the prognosis will improve, because they will reduce the build-up of damage to nerve cells.
That’s why we use DMDs after some cases of clinically isolated syndrome (CIS). After a CIS, if the patient has brain MRI lesions, they have a high risk of developing MS and we’ll give them DMDs. This will prevent or delay a second neurologic episode and, hopefully, the onset of multiple sclerosis.
There are different types of disease modifying drugs: some of them are more effective but also more aggressive. To find the best treatment we look at several things:
-
Factor #1: Course of MS
Most drugs are approved for recurring-remitent MS. Progressive MS is much trickier, and so far there is only one drug approved for it: ocrelizumab.
-
Factor #2: Efficacy
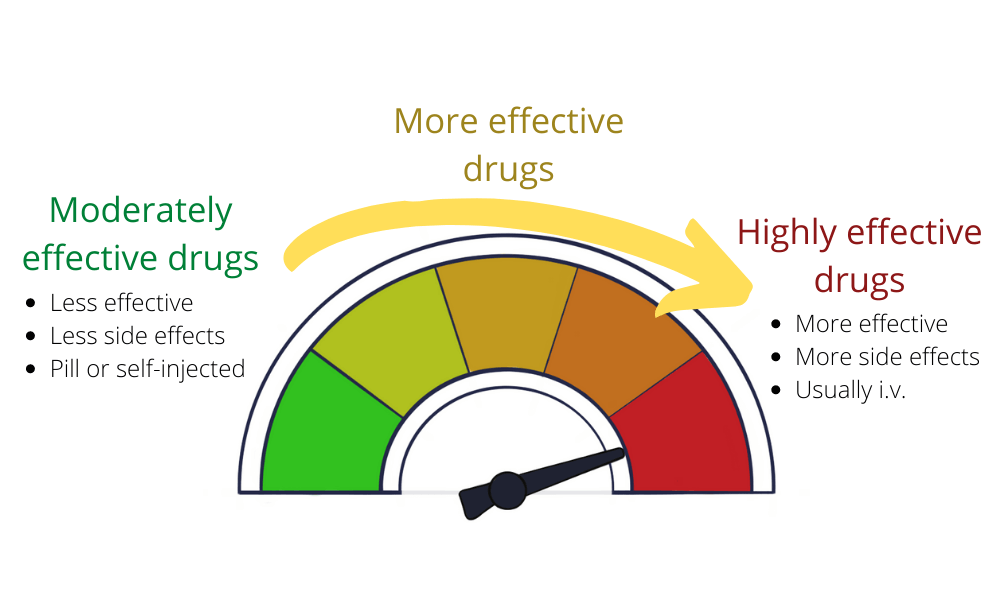
We classify DMDs according to their efficacy:
- Moderately effective: reduces relapses by about 30%
- More effective: reduces relapses by about 50%
- Highly effective: reduces relapses by about 70%
It looks like an easy decision, right? You may think: “why on earth wouldn’t I choose the highly effective?”.
Well, the more effective the drug, the more aggressive it is and the more side effects it has. So it’s a balance between how much disability your MS is causing and how much side effects you are willing to tolerate.
For example, some patients have such mild symptoms that they don’t even need treatment. If a patient has mild symptoms and needs some treatment, it doesn’t make sense to use the highly effective (and highly aggressive), because there is no need to take such a big risk.
-
Factor #3: Route Of Administration
Also, highly effective drugs are usually administered through i.v. drip in the hospital every month (sometimes every several months), which is a pain in the a## compared to simply taking a pill.
As for the other groups of treatment, it depends. Some of them you take as a pill and others as an injection. However, you don’t need to go to the hospital, you inject them yourself under the skin or into a muscle.
-
Factor #4: Side Effects
All drugs have some mild side effects like rash, gastrointestinal upset, flu-like symptoms, etc. However, when we choose highly-effective drugs there is an additional risk of some rare but serious side effects, like PML (progressive multifocal leukoencephalopathy), autoimmune disorders and blood clots.
– PML
PML is a terrible complication of some of the most effective MS drugs. It consists of an aggressive demyelinating disease that can happen in patients using therapies such as Natalizumab, Fingolimod and Dimethyl fumarate.
It affects patients with a John Cunningham (JC) virus infection. This virus doesn’t cause any symptoms in healthy people, so you may be infected and not know. Anyone can have it.
If it reactivates because of the drugs, however, it can cause motor deficits, visual symptoms, seizure… The prognosis is bad and many patients die before 1 year. Not all patients with the JC virus will develop PML, but there is a risk.
What we usually do is we test the patient for JC virus before choosing a therapy. If the patient is JC virus (-), there is no risk of PML. The patient will need periodic tests to confirm they don’t get infected. If the patient is JC virus (+), there is a risk for PML and it’s safer not to use those drugs unless we have no alternative.
You can see some examples of each group:
-
Moderately Effective
- Teriflunomide (Aubagio)
- Interferon beta 1a (Avonex)
- Interferon beta 1b
-
More Effective
- Fingolimod
- Cladribine
- Dimethyl fumarate
-
Highly Effective
- Natalizumab (Tysabri)
- Ocrelizumab
- Alemtuzumab
Sources
- Multiple Sclerosis Trust: https://mstrust.org.uk/
- National Multiple Sclerosis Society: https://www.nationalmssociety.org/
- Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/multiple-sclerosis/symptoms-causes/syc-20350269
Leave a Reply