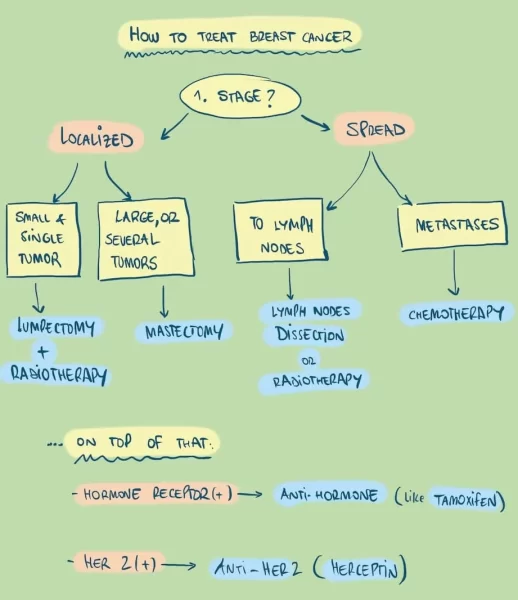
When it comes to treating breast cancer, we have several options.
Which one we choose will depend mainly on the stage: how much has the tumor spread? We don’t treat small tumors the same way as metastatic cancer. So let’s start with early stage tumors.
How to treat early stage tumors
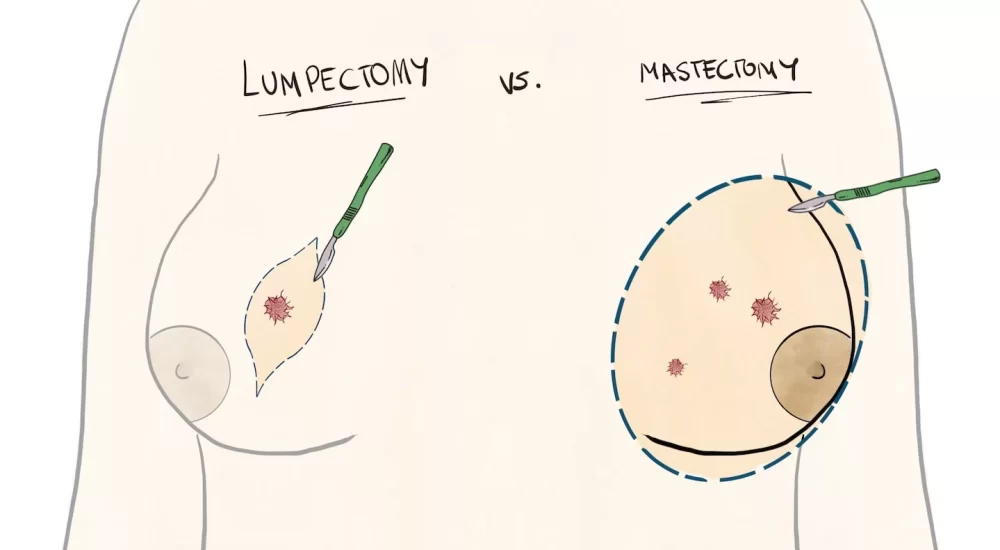
If the tumor hasn’t spread yet, the first step is surgery. We need to physically remove the tumor. To do that, there are two options:
- Lumpectomy: just remove the tumor. It’s a good option for small, single tumors.
- Mastectomy: removing the whole breast. We use it for larger tumors, or when there are several tumors.
Lumpectomy
Lumpectomy means removing just the tumor. We also call it breast conservation surgery and we use it for small single tumors. If the tumor is large or if there are several tumors, lumpectomy won’t do it and you’ll need a mastectomy.
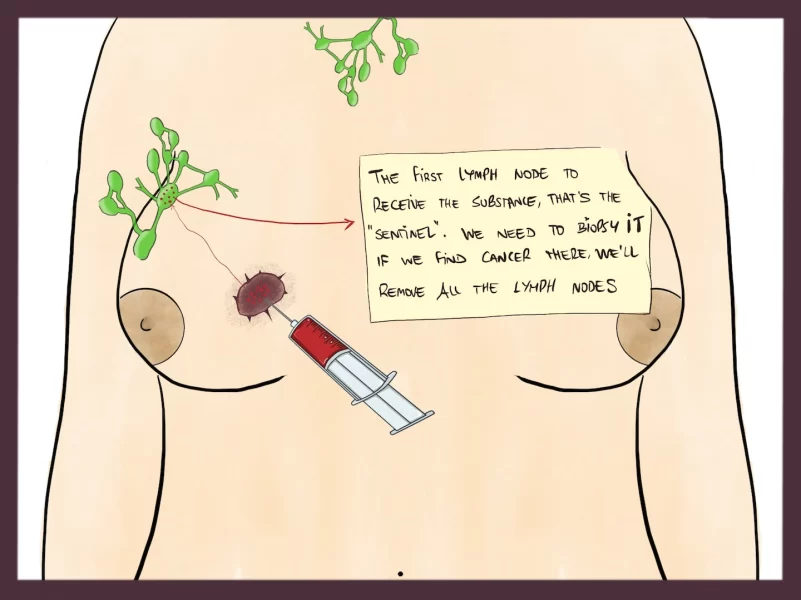
When your surgeon performs a lumpectomy, he must make sure your lymph nodes are ok, too. Because if there are affected, they’ll need to remove them too. To check your lymph nodes, doctors use a technique called lymphoscintigraphy or sentinel lymph node biopsy.
Why are lymph nodes important?
Lymph nodes are small nodes that take up lymph from a territory. The most important (around the breast) are the axillary lymph nodes. Then, the internal mammary and supraclavicular nodes.
See, the lymphatic system is like a highway for cancer. Once the tumor enters the system, it can travel easily from one node to the next, as if they were gas stations.
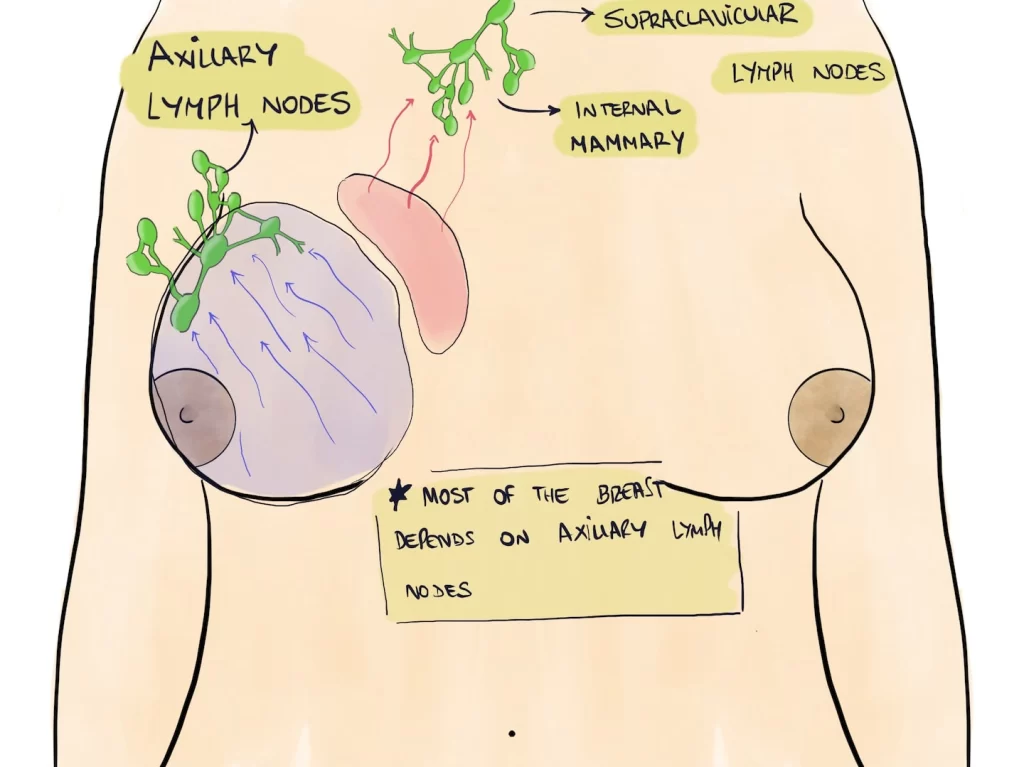
Some years ago, doctors would remove all the axillary lymph nodes, no matter whether they were affected or not. Just in case. However, some women developed lymphedema, a complication where the arm gets swollen and is prone to infections and wounds.
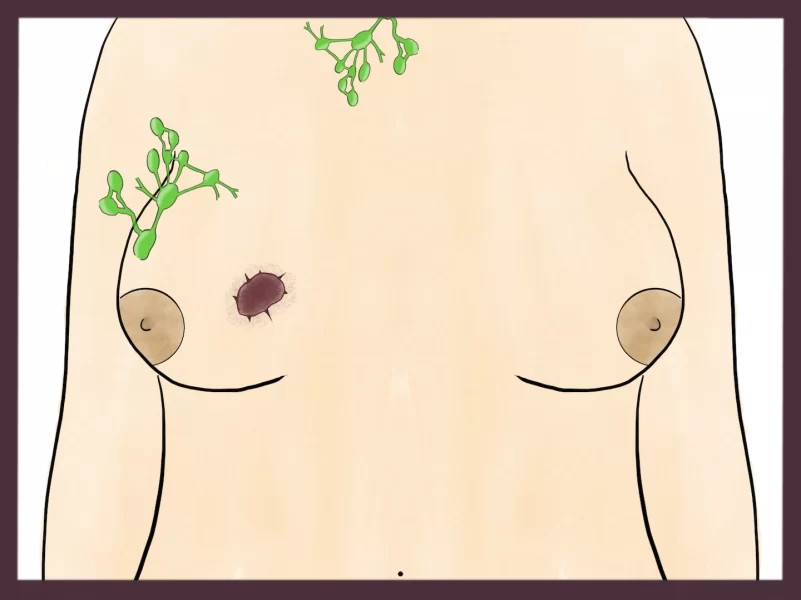
So they wondered: how can we find out which lymph nodes are affected?
The answer: lymph node mapping. This technique tells us which lymph nodes are more likely affected because they are closer to the tumor. It’s like finding the closest gas station to the robbery.
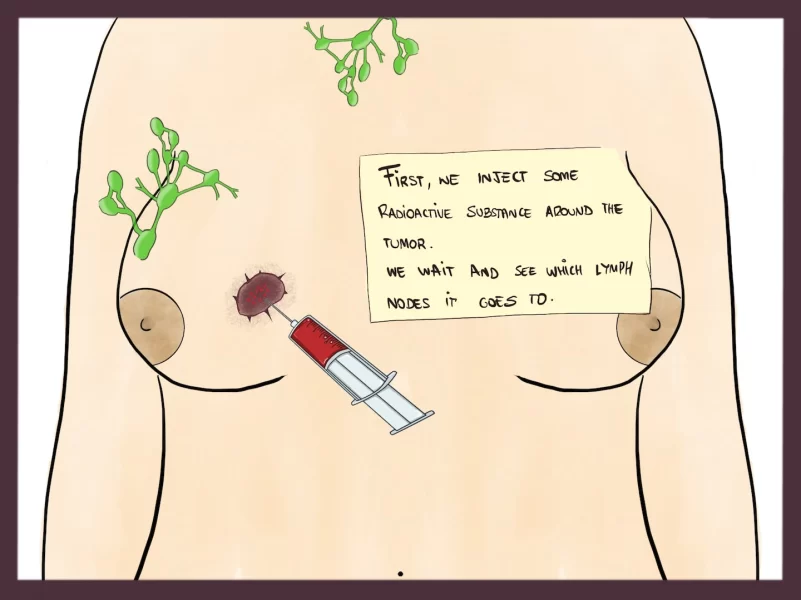
We inject a tracer into the tumor and see where it goes. The lymph node that gets the tracer, that’s the one we have to biopsy. If we find cancer there, we’ll remove those nodes. If we don’t, cancer hasn’t reached the lymph nodes yet and there is no need to remove them.
The sentinel lymph node technique goes like this:
After removing the tumor and (sometimes) they lymph nodes, there is radiotherapy. Most women need radiation therapy after a lumpectomy, to make sure there aren’t any malignant cells left.
Some women can’t have radiotherapy because they have skin disorders (like psoriasis or lupus) or because they already had radiotherapy in the same area. For these women, mastectomy is a better option.
Mastectomy
Mastectomy means removing the whole breast. It is a better option for:
- Large tumors, or several small ones
- Small breasts
- If for some reason, you can’t have radiotherapy
- When after several lumpectomies, margins are still positive (we can’t remove the tumor completely)
After mastectomy, you can have a breast reconstruction. Sometimes, they do it during the same surgery, either with implants or with fatty tissue. This fatty issue, they can get it from your belly, buttocks… In other cases, they place a tissue expander and reconstruct the breast later.
Radiotherapy
We use radiation to destroy malignant cells. Radiation damages the cell DNA, which causes the tumor to die. It’s good:
- After lumpectomy
- After mastectomy if the tumor is large or lymph nodes are affected
- For stage 4 cancer when we need to treat a single metastasis. Imagine you have one metastasis e.g. on your hip. You can’t remove it through surgery, but you can apply radiotherapy to it.
Radiotherapy can have some unpleasant side effects, like skin irritation and fatigue. For skin irritation, you should use loose clothes as well as some moisturizing cream. Also, don’t forget to drink lots of water. These side effects don’t start immediately, they take a few weeks.
After a couple of months, they improve and eventually go away.
Brachytherapy
In some places, they use brachytherapy after lumpectomy. Brachytherapy consists of several tiny seeds that go inside your breast, to the surgical bed (where they removed the tumor). These seeds are radioactive, so they release radiation around them. If there are any malignant cells remaining, brachytherapy will kill them.
Chemotherapy
As you may know, chemotherapy are drugs that kill malignant cells.
We use it in several cases:
- After we’ve removed the tumor. We call it adjuvant chemotherapy, and its goal is to destroy any malignant cells remaining.
- Sometimes, if the tumor is very large, we use it before surgery (we call it neoadjuvant). The goal is to try and shrink the tumor, so that it is easier for us to remove it through surgery.
- Finally, chemotherapy is our main weapon against metastatic cancer. If a woman has metastases in other organs, chemotherapy is a good option because it will reach all those organs. Afterwards, she can also have radiotherapy or hormone therapy, depending on the case.
Hormone therapy
Breast cancer has some special features. For example: breast cancer can respond to hormones. If your tumor has hormone receptors on its surface, it will grow faster when there are hormones around it.
So, it’s important to find out if your tumor is “hormone receptor positive (+)”. If it is, there are some drugs that will help.
Some of these drugs reduce the levels of hormones in your body, like goserelin. Less hormones, less cancer growth.
Another type are selective estrogen receptor modulators (SERMs), like tamoxifen. These drugs look like estrogen, but they are not, so they take estrogen’s place and prevent its action.
Because they mess with your hormones, they can have some side effects, like hot flashes, night sweats and vaginal dryness.
Hormone therapy usually lasts 5-10 years.
Anti-HER2 therapy: Herceptin
Some tumors display HER2 receptors, and we can also target these receptors. The most well-known anti-HER2 drug is Herceptin (= trastuzumab).
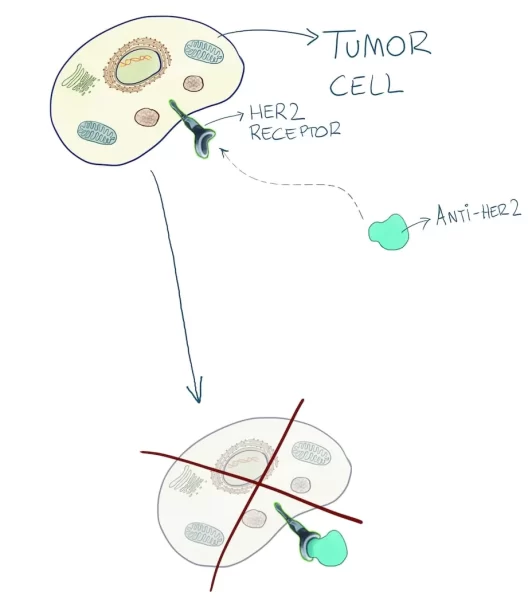
In the past, HER2 tumors had a gloomy prognosis because they are, in fact, more aggressive. But now, with Herceptin, their prognosis has really improved.
We can use Herceptin as an adjuvant treatment, after surgery. Also, we can use it for metastatic HER2 + cancer.
Herceptin can have some side effects. The most important one is cardiotoxicity: it can worsen your heart function. It doesn’t happen to all women, so you’ll need to have regular cardiac checkups before, during and after using it.
To sum it up, breast cancer treatment looks like this:
Leave a Reply