By the time we diagnose ovarian cancer, it usually has grown outside the ovary already, usually in the form of (ascites). In these cases, we must be really aggressive with our treatment.
[box type=”shadow”]
Table of Contents
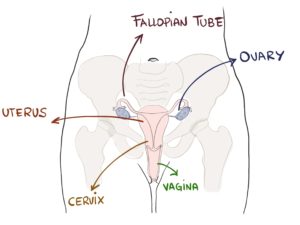
What are the ovaries?
The ovaries are part of the reproductive system in women. They store the eggs, releasing one every month to allow for fecundation.
When ovarian cancer starts growing, it is small and doesn’t cause any symptoms, which is not so good, because it makes it hard for us to detect it at an early stage. Only when it grows and infiltrates the pelvis it starts causing symptoms.
By the time we diagnose ovarian cancer, it usually has caused ascites (fluid in your pelvis), with discomfort and a “stuffed” feeling. That’s the most frequent situation: most women find out they have ovarian cancer when they already have ascites.
What causes ovarian cancer? Risk Factors
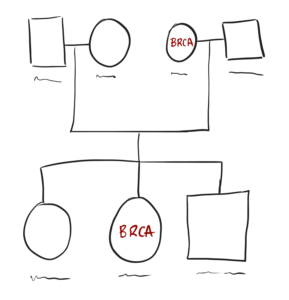
Being a woman (of course) and age: older women have higher risk. Also, there is a family component: if other women in your family had ovarian cancer, then you have a higher risk. This is especially true if there is a BRCA mutation in your family. Those carrying the mutation will have an increased risk for breast and ovarian cancer. Around 1 out of 10 cases of ovarian cancer are caused by BRCA mutations.
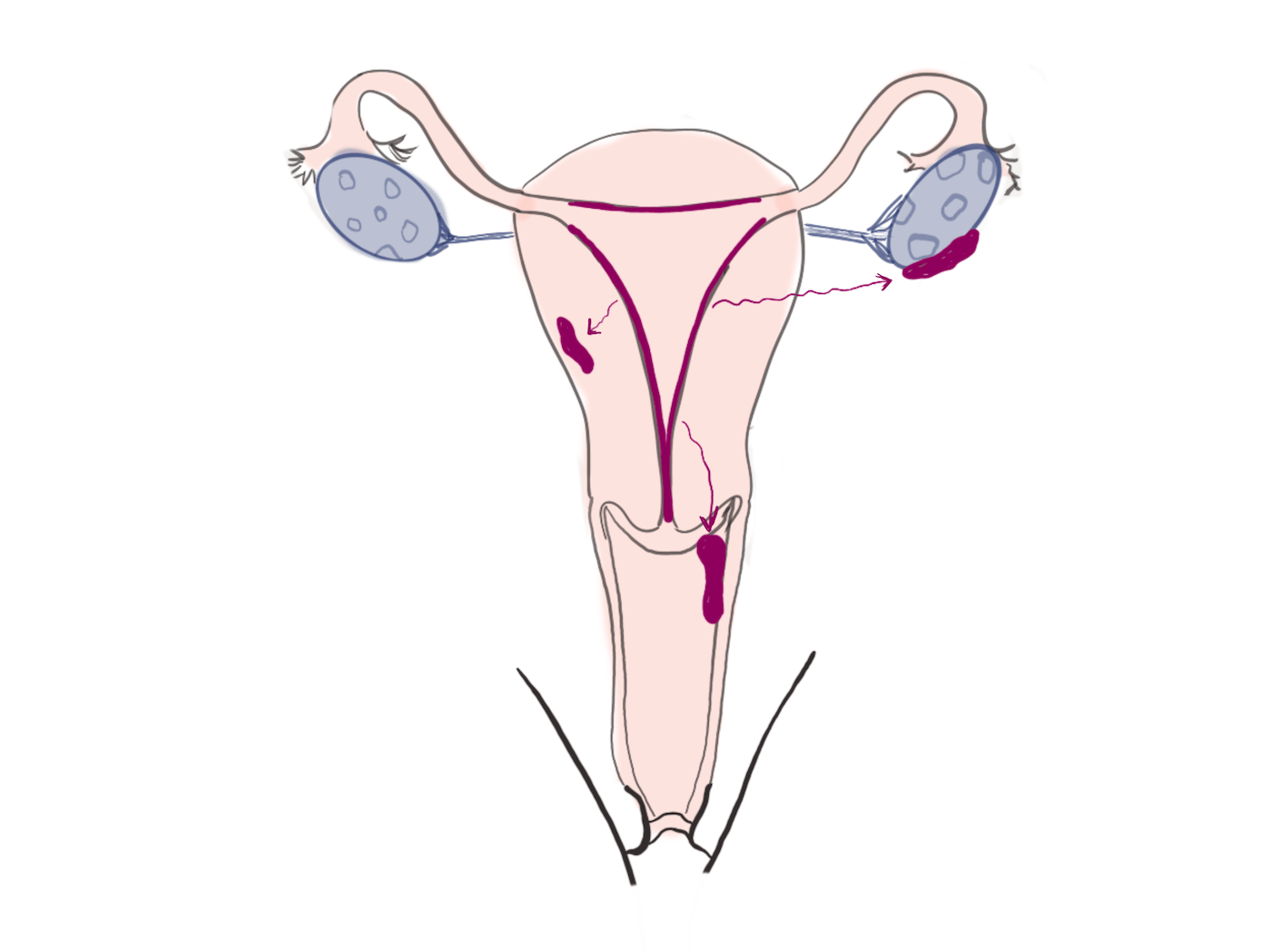
Women who suffer endometriosis have a higher risk, too. Endometriosis is a disorder in which there is endometrial tissue outside the uterus, usually in the ovaries. Those affected ovaries can develop cancer.
Finally, an unhealthy lifestyle, like smoking, obesity and lack of exercise also increases the risk for ovarian cancer.
What are the symptoms of ovarian cancer?
Ovarian cancer is usually silent at the beginning. It doesn’t cause any trouble until it has spread to the pelvis, filling it with fluid. By then, you can start to feel some symptoms, like feeling bloated or pelvic pain. Also, some women feel they can’t anything or the need to pee too often.
There are some other less common symptoms, like pain during sex (dyspareunia), fatigue or weight loss.
How do you diagnose Ovarian Cancer?
The first tests are: blood marker CA-125 and ultrasound (U.S.). CA-125 is a marker that rises when there is an ovarian cancer. However, it is not perfect, and it can be:
- Normal despite having cancer (false negative test)
- Elevated despite not having cancer (false positive)
That’s why we must interpret it together with other tests. It’s also useful for follow-up: if it rises after we’ve removed the tumor, it may mean there is recurrence, cancer has come back.
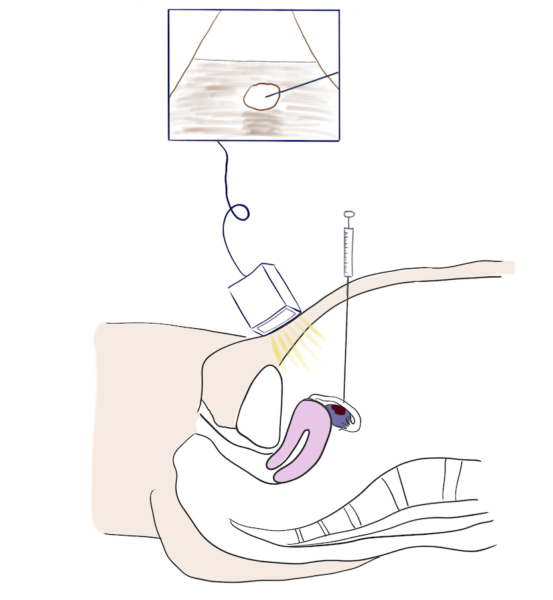
Then we have U.S. We can perform the U.S. through the abdominal wall or through the vagina. Gynecologists are the ones to perform transvaginal U.S. usually. It allows a better view of the uterus and ovaries. U.S. gives us a first impression on whether the ovaries have any masses on them. U.S. can also detect ascites, which is a common presentation for ovarian cancer. If we find a suspicious mass, we we need to get a biopsy to make sure it is cancer (you don’t want to give chemotherapy or remove her ovaries without being sure).
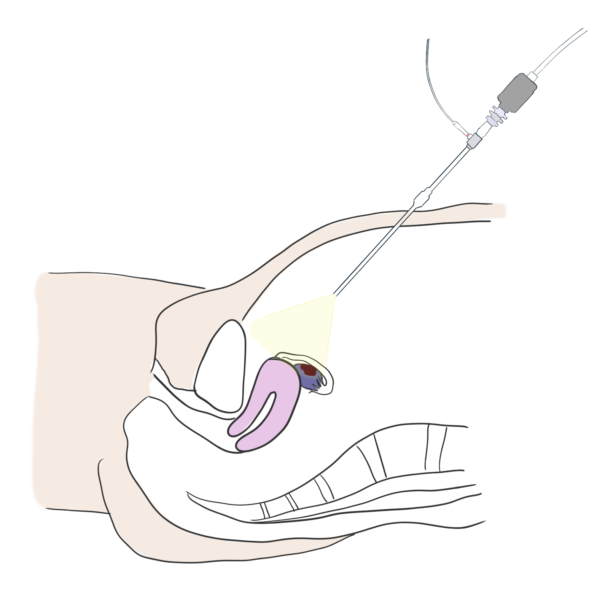
We can perform the biopsy percutaneously or through laparoscopy.
In a percutaneous biopsy we insert a needle through your abdomen with the help of U.S. images. We pierce into the mass and get a sample. It’s the least aggressive option and only requires local anesthetics.
Laparoscopic biopsy, on the other side, consists of several rigid tubes that go into your abdomen. Through those tubes the doctor will insert a camera to see everything from inside. Also, they will get tools inside to take the sample. This option does require general anesthesia.
Has the tumor spread? Staging
Then we must get to know how much the tumor has spread.
- Is it affecting one ovary? Both ovaries?
- Is there ascites?
- Are there distant metastases: to the bone, liver, lungs…?
A full body CT is the best way to get this information. It is like a 3D x-ray that shows the whole body inside. Staging is crucial as we will choose different treatment strategies depending on staging. For example, if it’s only a tiny nodule inside the ovary, removing the ovary may be enough. On the other side, if the tumor is infiltrating or there are metastases, you will probably need aggressive surgery and chemotherapy.
To stage a tumor, we give it a number from I to IV. “I” means it has not spread and “IV” means there are distant metastasis.
- I: tumor only affects the ovaries. There are several subgroups: IA means only one ovary is affected. IB, both ovaries. And IC if there is fluid/ascites in the pelvis.
- II: extension to the pelvis. For example, the tumor is invading the uterus, cervix, fallopian tubes…
- III: there is extension to the rest of the abdomen. They are called peritoneal implants.
- IV: there are metastases. They may affect the bones, liver, lungs…
How do you treat ovarian cancer?
As we said, depending on the staging we will need one therapy or another. First thing we must know is whether cancer has spread.
When cancer hasn’t spread
If there is only 1 ovary affected and the woman is young, we can remove only the affected ovary. This is called oophorectomy, and it will allow you to have children in the future, by keeping the other ovary and uterus.
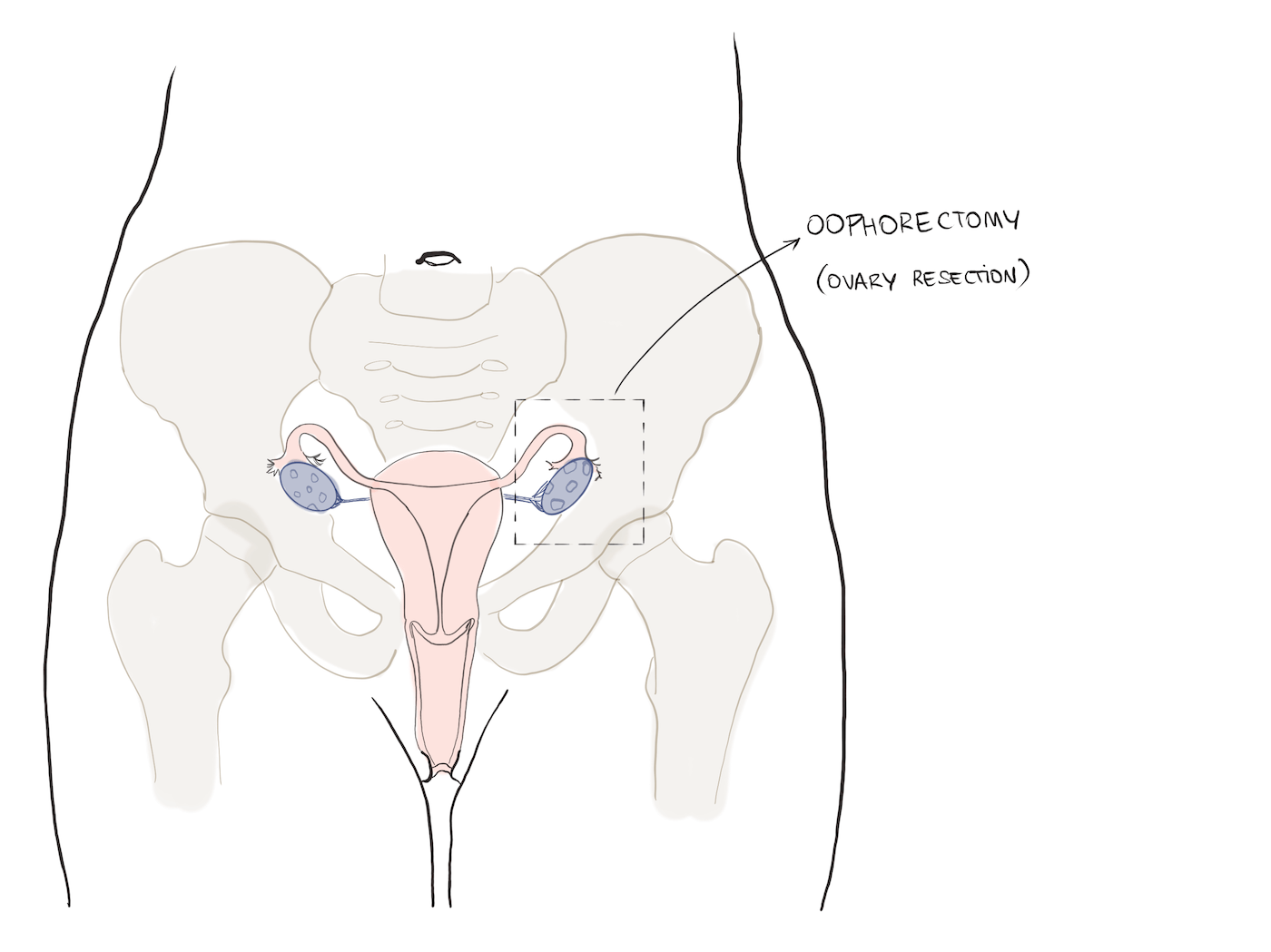
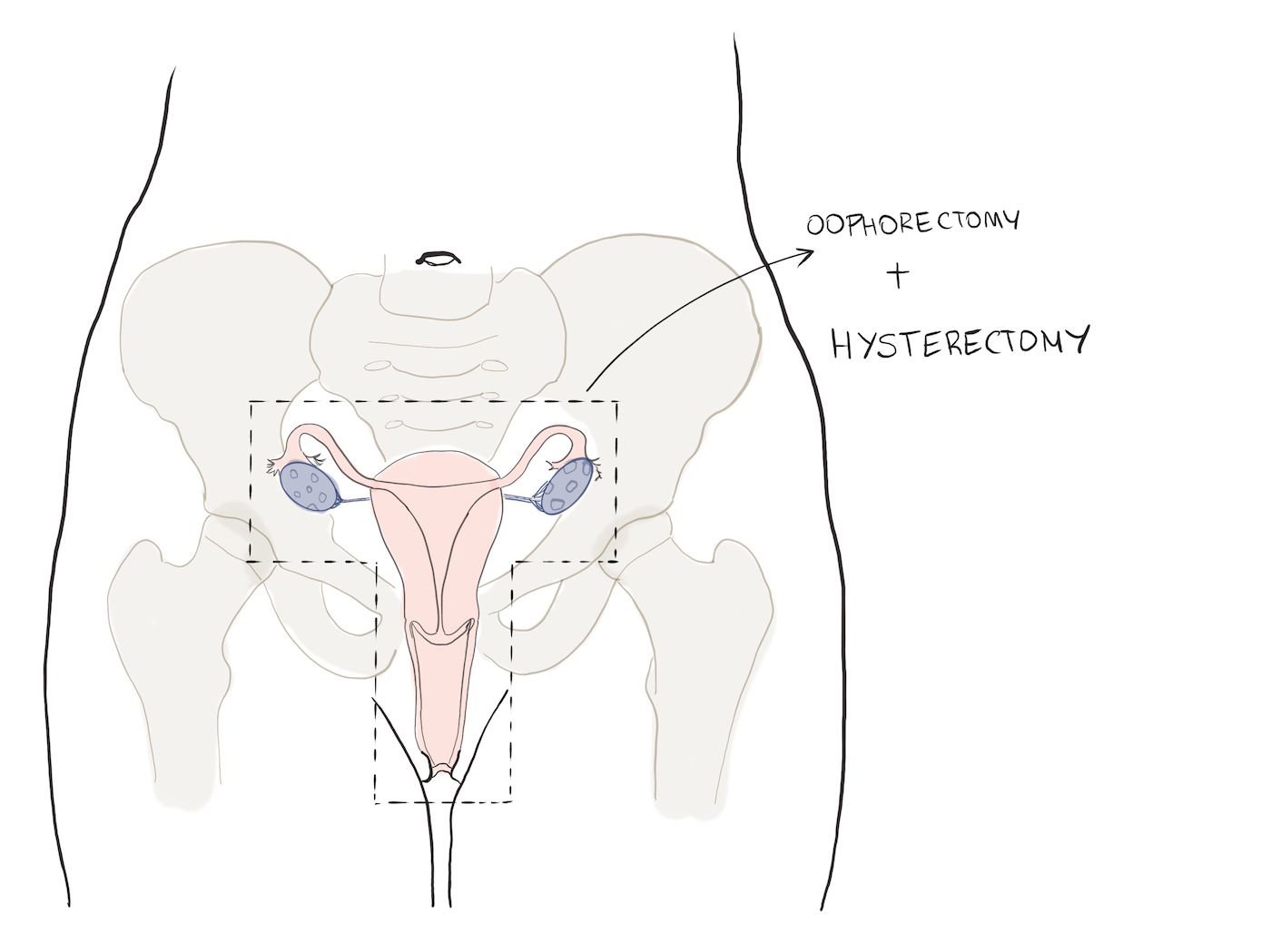
If the stage is higher you will need a “double anexectomy + histerectomy”. That means removing both of your ovaries and your uterus.
After that, your doctor will have to decide if you need chemotherapy. There is usually a multidisciplinar committee formed by a gynecologist, oncologist… that make those decisions together.
When cancer has spread…
This is the most common scenario. Most ovarian tumors are at an advanced stage by the time we detect them. The best treatment here is usually a mix of surgery + chemotherapy.
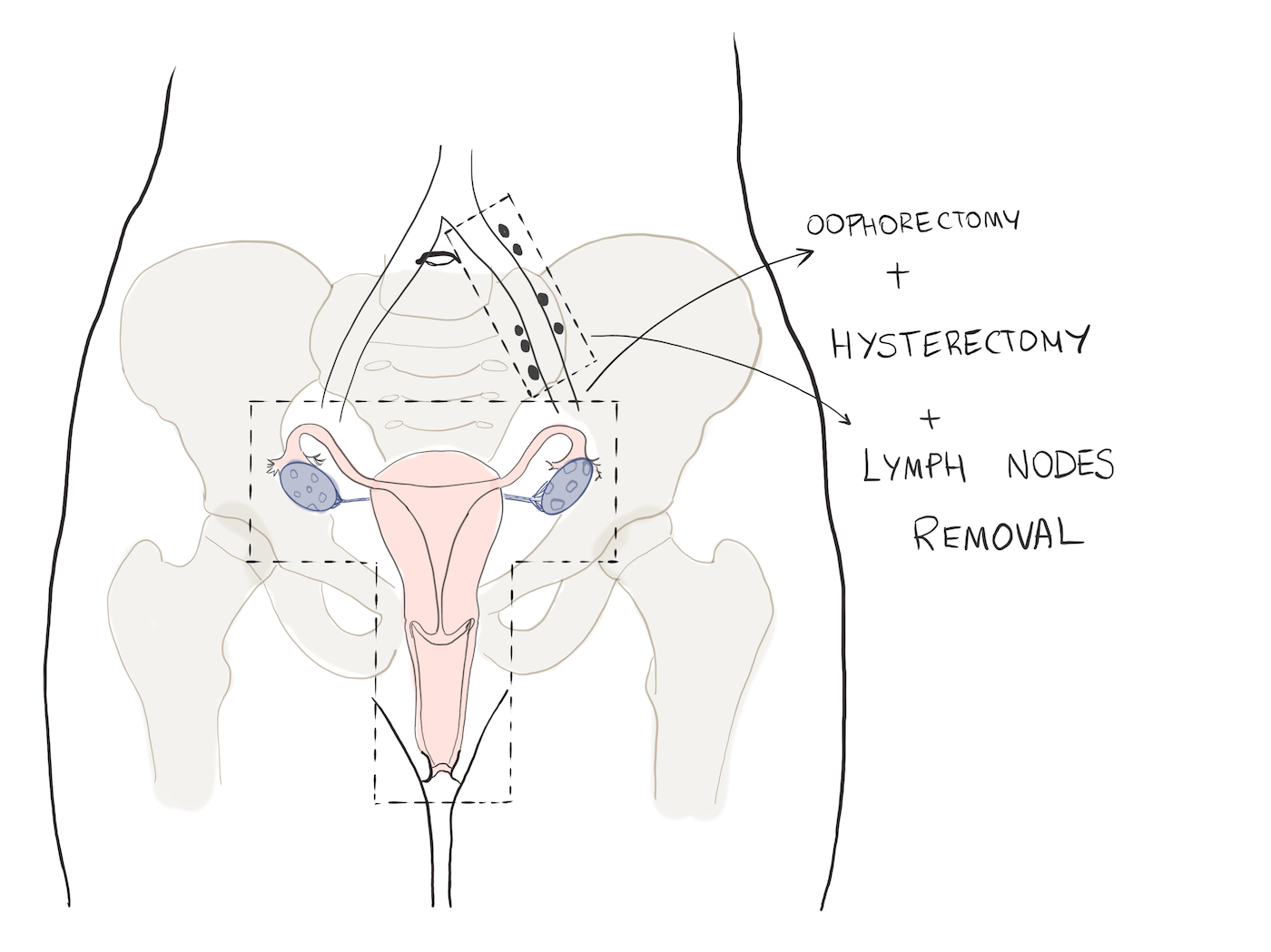
Surgery
Surgeons will remove the uterus and both ovaries and also peritoneal implants if possible. Sometimes they will perform debulking surgery, which is they will try to remove as much malignant tissue as possible, even if they can’t remove all of it. With other types of cancer (lung, liver…) if you can’t remove the whole tumor, it is not worth operating, because it will come back.
With ovarian cancer it’s different though. Surgeons try to remove as much tumor as possible. If there are 10 implants and you remove 8 of them, the prognosis gets better. After that, you can use other therapies like chemotherapy or radiotherapy.
Chemotherapy
We can use chemotherapy in several ways: First, we can use it before surgery, to shrink lesions (this is called neoadjuvant chemotherapy). We can also use it to treat metastasis. Finally, we can use it after surgery (adjuvant chemotherapy), to reduce the chances that cancer will come back (recurrency).
Intraperitoneal chemotherapy
Ovarian cancer allows for a suprising way to use chemotherapy. The problem with peritoneal implants is they are hard to remove. Surgery will remove the large nodules but there will always be some microscopic cells remaining. Regular chemotherapy is good for spread cancer, but it penetrates very poorly into the peritoneum. So some time ago, somebody thought: what if we apply chemotherapy directly into the peritoneal cavity? And that’s how these techniques were born:
- Hyperthermic intraperitoneal chemotherapy (HIPEC)
- Early post-operative intraperitoneal chemotherapy (EPIC)
They consist of placing chemotherapy inside your abdomen, so that they surround the peritoneal implants and kill tumoral cells. To be effective implants must be very small, around 2 mm at the most. That’s why it’s important to remove larger implants through surgery.
Questions and answers
-
Are ovarian and breast cancer related?
Sometimes they are. For example if you carry a BRCA mutation you’ll be at risk for both ovarian and breast cancer. It doesn’t mean that you’ll have both necessarily, but your risk will be higher.
-
Can ovarian cancer cause weight gain?
Yes, it can. Even though cancer usually causes weight loss, ovarian cancer can cause both: weight loss or gain. You can gain weight because of ascites: the fluid accumulating in your abdomen can give the impression that you are gaining weight.
-
Where does ovarian cancer metastasize?
Typically to your pelvis and abdomen, causing ascites and peritoneal implants. If it keeps spreading, it can travel anywhere: your liver, lung, brain…
Leave a Reply