Prostate cancer is one of the most common cancers in men: 1 out of 8 men will have it at some point in their lives.
Fortunately, most of them grow slowly, which gives us time to treat it. However, few men are aware of the different ways they can treat their cancer. Most know about surgery, yes. But there are other options, like radiation therapy.
One alternative is radiation therapy, a non-invasive approach that offers good results while reducing some of the side effects of surgery.
What is Radiation Therapy?
Radiation therapy uses high-energy X-rays to burn and kill cancer cells. We use it to treat several types of cancer, including prostate cancer.
It’s non-invasive, effective, and has fewer side effects than surgery. Hence, it’s an excellent alternative to surgery.

There are 2 different types of radiation therapy:
· External Radiation: an external beam is directed towards the tumor. You need this therapy every day for several weeks until your whole prostate is “fried.” Each session is quick and painless. This is the one we’ll cover in this post.
· Brachytherapy: you’ll get some tiny radioactive seeds inside your prostate. Those seeds release radiation from within the prostate, which will kill cancer cells while leaving the surrounding tissues intact. You can read more here.
What are the goals of radiation therapy?
We can use it before, after, or instead of surgery, depending on our intentions.
- As a standalone therapy. We use it instead of surgery, trying to cure the patient by burning the whole tumor. We use it for early-stage tumors.
- Neoadjuvant therapy: Imagine you have a tumor, but it’s too large to remove through surgery. Then one way to solve it is by trying to shrink it through radiation. If it does get smaller, your surgeon will then remove it.
- Adjuvant therapy: after they remove your prostate, you can also get radiation. In this case, the goal is to try and burn any remaining cancer cells. It’s used for aggressive tumors, reducing the chances that the tumor will grow back.
- Palliative care: If cancer has spread to other organs radiation can still be useful. Even though it won’t cure the patient, we can use it to relieve symptoms and improve his quality of life. For example, imagine your tumor has spread to your bone, to your vertebra, causing you a lot of pain. Radiation allows us to reduce that lesion and improve your pain.
What is the process like?
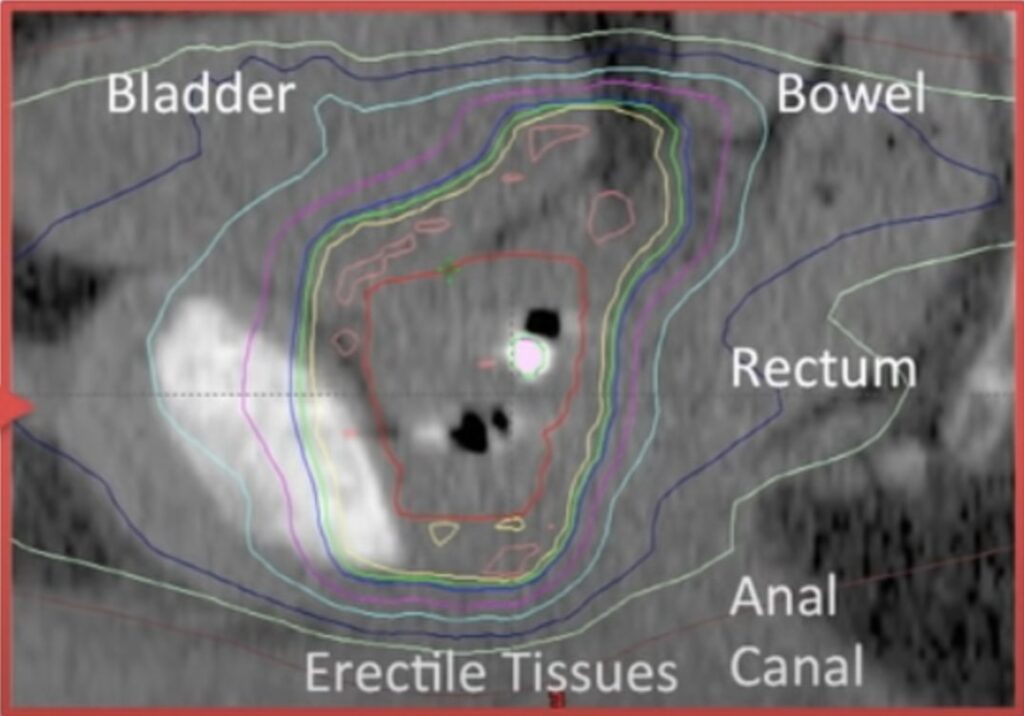
- First comes planning. A radiation team will use an MRI to map your prostate and surrounding tissues. Then, they will create a customized plan for you, detailing:
- What’s the right dose for you
- How many sessions you’ll need
- Which angles they’ll use to target your prostate
- Simulation: You will lie on the treatment table as if being treated. That way, they make sure they are targeting the right area.
- Treatment Sessions: Normally, you’ll need daily sessions, Monday through Friday, for several weeks. Each session lasts for around 10-30 minutes. The radiation time, though, is around 5 minutes, while the remaining time goes to positioning, preparing everything and so on.
During each session, you’ll lie on the table while a machine delivers radiation to your prostate. It doesn’t hurt. In fact, you won’t feel a thing.
Side effects
The most common side effects of radiation therapy are:
Urinary problems
You may feel that you need to pee more often. Then, some people have an urgency to pee (you need to pee right now). Other people, however, have the opposite problem: they can’t start peeing when they go to the toilet.
Because of the irritation, you can get a burning sensation while you pee.
Bowel problems
Because your rectum is right next to the prostate, you can get diarrhea, rectal discomfort and blood in your stool.
Fatigue
Many patients suffer from fatigue, which can be mild to moderate. It usually lasts for several weeks after treatment ends.
Sexual Dysfunction
You can get erectile dysfunction, which means you can’t get hard. In some cases, it’s temporary; in others, it’s permanent. You can read how to treat it here.
Also, you can have trouble with your libido (not interested in sex).
Finally, some men have changes in orgasm or ejaculation.
Skin reactions
The skin in your pelvis may get red, dry, and irritated.
How to choose between radiation therapy and surgery
If your cancer is early stage, you may consider whether surgery or radiation is better for you.
Here are some general guidelines:
| Guidelines for choosing | Surgery (Prostatectomy) | Radiation Therapy |
| Cancer Stage and Grade | Typically for early-stage (localized) prostate cancer. | An option for localized and locally advanced cancer. |
| Tumor Characteristics | For less aggressive tumors. | Suitable for more aggressive tumors |
| Health and Age | Suitable for younger, healthier patients. | Preferable for older patients or those with other diseases. |
Leave a Reply